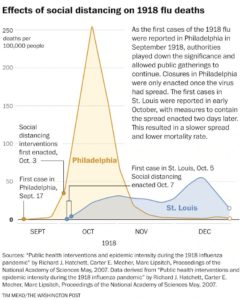
It’s hard to think about anything good coming out of this pandemic. Every story of a life lost is heartbreaking. Like you, I have shed many tears in the past month as I read and heard their stories.
And yet, it is encouraging to consider some of the positive changes we may see when we get to the other side of this crisis and are living and working in the “new normal”. We don’t yet know when that new normal time will come. But there are changes in healthcare and how we work that will hopefully be long lasting. I’m not talking about the overall healthcare system or macro societal and economic changes – I’ll leave that to others.
From a health IT lens, here’s my take on some of the positive changes:
Telehealth – There is no question that this crisis has led to a huge increase in telehealth and new use cases. Some organizations are seeing 50+ times the number of telehealth visits compared to before. With regulations relaxed and no alternative, telehealth is being used in many different scenarios. Training, broad deployment and adoption has accelerated as clinic visits are cancelled and telehealth becomes the primary means to connect with your physician. And on the frontlines of COVID-19 hospital care, leveraging it with inpatients to protect staff and reduce the amount of PPE used has also become common. We’ve reached the tipping point for telehealth and I expect we’ll see it continue to grow in the future. A recent article in NEJM Catalyst by Judd E. Hollander, MD, and Frank D. Sites, MHA, BSN, RN, titled “The Transition from Reimagining to Recreating Health Care Is Now”, covers how organizations need to look at expanded telehealth use post COVID-19.
Rapid deployment – From an IT perspective, supporting the effort to stand up a field hospital or alternate care site such as the 1000 bed Boston Hope Medical Center is like a “greenfield” hospital compared to rolling out a new EHR and the associated infrastructure at an existing hospital. What lessons can be learned and applied from these rapid deployments when it comes to getting all hospitals in a healthcare system on a common platform? Does it have to take years?
Interoperability – I use this term loosely here. New York considers all hospitals statewide as one system to share resources and staff. The Hospital for Special Surgery (HSS) in New York City quickly transitioned from an orthopedic only hospital to take other surgical cases and COVID-19 patients, credentialing physicians and providing access to systems. While state and regional Health Information Exchanges (HIEs) have varied in their successes over the years and physician credentialing is one of the slowest and most tedious administrative processes in healthcare, it gives me hope to see how effectively and quickly hospitals are working together in a time of crisis.
Workflow changes – With EHR systems it can often take weeks or months to identify requirements, reach consensus, make the changes, test, train, and implement. Those changes are now measured in hours or days if it’s needed for COVID-19. IT teams and their clinical partners should ask what processes can be streamlined when we are in the new normal. Continue reading